Could the Key to a Long Life Be In These Little Devices?
Knowledge is power, but action is necessary to put that knowledge to use. We know the keys to a long life from research on the world’s longest-living populations. Meanwhile, modern life is pulling us further away from these healthy habits. Fortunately, a modern solution may also help us truly take action towards living a long life.
Wearables are seen by many as a great possibility for building healthy habits into our daily lives. A wearable device incorporates technology into something you wear such as clothing or an accessory (think Apple Watch, Fitbit or Google glass). They always make me think of James Bond!
A PWC study found that consumers see great potential with widespread use of wearable health technologies for long life and better health:
- 56% believe life expectancy will grow by 10 years because of wearables
- 46% believe they will decrease obesity
And, the potential for these devices being integrated into a healthy, long life is amazing! Cisco estimates the number of wearable devices in use will jump to almost 177 million by 2018.
The advantage of wearable health technologies is the ability to get real-time data that we can use to change behaviors and prevent disease (before we see symptoms, when reversing damage becomes much more difficult). Seventy-one percent of Americans claim that wearable technologies have improved their overall health. By bringing the data right into our daily lives (it can’t get much more convenient than wearing it), people tend to be more accountable for their personal health and fitness, all of which can lead to a long life and less illness. There are devices that remind you to take medicines or keep up with healthy habits (fitness especially), help track nutrition, monitor/correct posture and more.
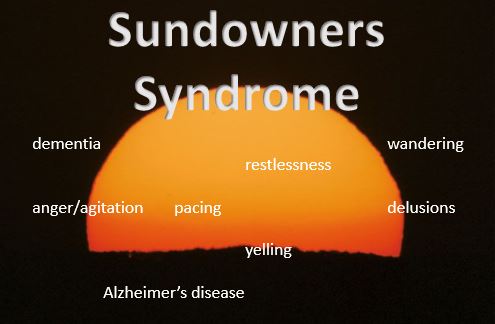
Wearable technology has the potential for a big impact on healthcare. Right now, a doctor’s interaction with patients is mostly limited to the office visit which gives the doctor a very small window into the daily life of the patient. Wearable technology can monitor key vital signs and send measurements of important data to the patient, caregivers and medical providers. Wearables also have enormous potential for research purposes.
The Best Fitness Wearables for a Healthy, Long Life
The Jawbone is a reasonably priced option that covers the basic measurements and features you’d want in a fitness tracker. Simply slip it on your wrist and track: activity (steps, calories burned and bursts of activity), sleep mode (tracks sleep time and quality and offers a smart alarm to wake you more easily during the best part of your sleep cycle) and a stopwatch you can set for timing exercise.
The Misfit Flash is a great option for first-timers and the budget-conscious, coming in at about $25-30. This wearable offers all the typical tracking you’d expect (sleep, steps/activity) but also does well timing various types of activity such as swimming and even sports. The Xiaomi Mi Band has gained incredible popularity in China, and is now available outside of China, as an ultra-affordable option. Get it on Amazon for as little as $18-27.
For those who want to monitor their heart rate, the Fitbit Charge HR is a great option. While covering the usual activity tracking, this one also does a great job as a heart rate monitor/tracker (and has a nice app with the ability to set challenges for yourself). You can also log food with a bar code scanner, food database and calorie counter.
Garmin also has a range of sophisticated options.
Stay tuned for more about all kinds of unique wearable health technologies and ways tech is changing healthcare, caregiving and our access to a healthy, long life. Sign up for our newsletter so you never miss out!










 Popular Downloads
Popular Downloads


 Get Our Newsletter!
Get Our Newsletter! Mission Statement
Mission Statement

